Pancreatic Cancer
For Patients
Pancreatic cancer is relatively uncommon, accounting for only 2.5% of all cancer cases in Australia. Therefore, some people may not fully understand the role of the pancreas and how cancer can develop here. This section outlines the functions of the pancreas, as well as important information about pancreatic cancer, including possible causes, diagnosis and treatment.
Causes of Pancreas Cancer
Unfortunately, little is known about the exact causes of pancreatic cancer, so it can be difficult to explain why some people get the disease and others don’t. Some of the few known risk factors are outlined below.
Pancreatic Cancer is a Genetic Disease
Pancreatic cancer is caused by mutations or changes in a person’s DNA. These genetic mutations may be inherited, meaning that we are born with them, or they may be acquired throughout a lifetime. In most cases of pancreatic cancer, mutations are caused by environmental, lifestyle and aging factors. Approximately 5-10% of all pancreatic cancers are the result of inherited changes, which explains why pancreatic cancer appears to run in some families.
The acquired changes (changes that develop after we are born) can occur when mistakes are made when a cell replicates or divides. Cells in the body are continuously replicating in order to make new cells and replenish cells, which have died as part of the normal cell cycle. This process is regulated by DNA. When DNA is damaged, changes occur in these instructions and as a consequence may result in abnormal growth, such as a tumour.
Certain risk factors can also increase a person’s chance of acquiring these genetic changes, which can lead to the development of pancreatic cancer.
Risk factors
Some of the known risk factors are:
Smoking
Exposure to cancer causing chemicals (carcinogens), such as those found in cigarette smoke, can significantly increase a person’s risk of pancreatic cancer. Tobacco smoking is a major risk factor, and those who smoke or have smoked are approximately two to three times more likely to develop cancer of the pancreas.
Age
The incidence of developing pancreatic cancer increases dramatically with age. About 80% of cases occur in people between the ages of 60 and 80.
Nutrition and Dietary factors
Diets with a high intake of meat and/or saturated fat, and a reduced intake of fruits and vegetables can increase the risk of pancreatic cancer.
Other dietary factors associated with a greater risk of cancer of the pancreas include:
- Foods high in cholesterol
- Increased consumption of salt and smoked meats
- High intake of dehydrated and/or fried foods
- Over consumption of barbecued meat (exposure to the carcinogen heterocyclic aromatic amine [HCA])
Environmental
Those who are frequently exposed to certain pesticides and petroleum products may have an increased risk of pancreatic cancer. High rates of pancreatic cancer have been noted among industrial workers; for example the chemical manufacturing and metal industries.
Medical Conditions
Chronic pancreatitis
Patients who have chronic pancreatitis are 5 times more likely to develop pancreatic cancer. Chronic pancreatitis is characterised by recurrent inflammation of the pancreas. The most common cause of chronic pancreatitis is long-term alcohol abuse.
Diabetes Mellitus
There is a long-standing association with Diabetes Mellitus and an increased risk of developing pancreatic cancer. The explanation as to why this is the case is not well understood, thus further research is being conducted in order to understand the connection between cancer of the pancreas and Diabetes.
Previous surgery – Gastrectomy or Cholecystectomy
There appears to be an increased risk of developing pancreatic cancer in those who have had certain types of surgery, such as a gastrectomy (portion of stomach removed) to treat stomach ulcers for example, or those who have had a cholecystectomy (gallbladder removal). There are specific types of bacteria that can produce carcinogenic chemicals called nitrosamines as a result of these types of surgery, which may increase the risk of pancreatic cancer.
Hereditary Aspects of Pancreatic Cancer
The majority of pancreatic cancers occur by chance, however 5-10% of pancreatic cancers are inherited. Genetic mutations can be passed down through families, causing some individuals to be born with an increased susceptibility to pancreatic cancer. Although the majority of genes responsible for this inherited risk remain unknown, there are a number of genetic disorders associated with an increased risk of pancreatic cancer. These include:
Breast Cancer Gene 2 (BRCA2)
Mutations in the BRCA2 gene are generally associated with hereditary breast and ovarian cancer. However, BRCA2 mutations may also account for 6-16% of hereditary pancreatic cancer cases. It is estimated that the lifetime risk of developing pancreatic cancer for those carrying a BRCA2 mutation is 5%.
Peutz-Jeghers Syndrome
This syndrome is caused by mutations in the STK11 gene. It is associated with the growth of polyps (usually benign) in the stomach and intestines, and pigmentation on the lips and nose. The lifetime risk of developing pancreatic cancer is 36%.
Hereditary Pancreatitis
Hereditary pancreatitis is rare and can be caused by mutations in the PRSS1 or SPINK1 gene. This condition is characterised by frequent episodes of chronic pancreatitis (long-term inflammation of the pancreas) beginning from a relatively young age. The lifetime risk of developing pancreatic cancer is estimated to be as high as 40%.
Familial Atypical Multiple Mole Melanoma (FAMMM)
FAMMM is caused by mutations in the CDKN2A gene, and affected individuals tend to develop a large number of skin moles and melanomas at young ages. They may also be susceptible to cancer of the pancreas, however this increased risk has not been confirmed in an Australian population.
Lynch Syndrome or Hereditary Non-Polyposis Colorectal Cancer (HNPCC)
Lynch syndrome is an inherited predisposition to developing bowel cancer, due to mismatch repair gene mutations (MLH1, MSH2, MSH6, PMS2). It is also associated with an increased risk of other cancers, including stomach, endometrial, ovarian, and pancreas cancer.
Familial Adenomatous Polyposis (FAP)
FAP is characterised by multiple colorectal adenomas at a significantly younger age. Benign and malignant tumours can also be found in other sites, such as the duodenum, stomach and skin. FAP is a result of mutations in the APC gene and is associated with an increased risk of pancreatic cancer.
It is important to note that having one or more of these risk factors, medical and/or genetic conditions does not mean someone will develop pancreatic cancer. Individuals concerned about their personal risks should consult with a doctor.
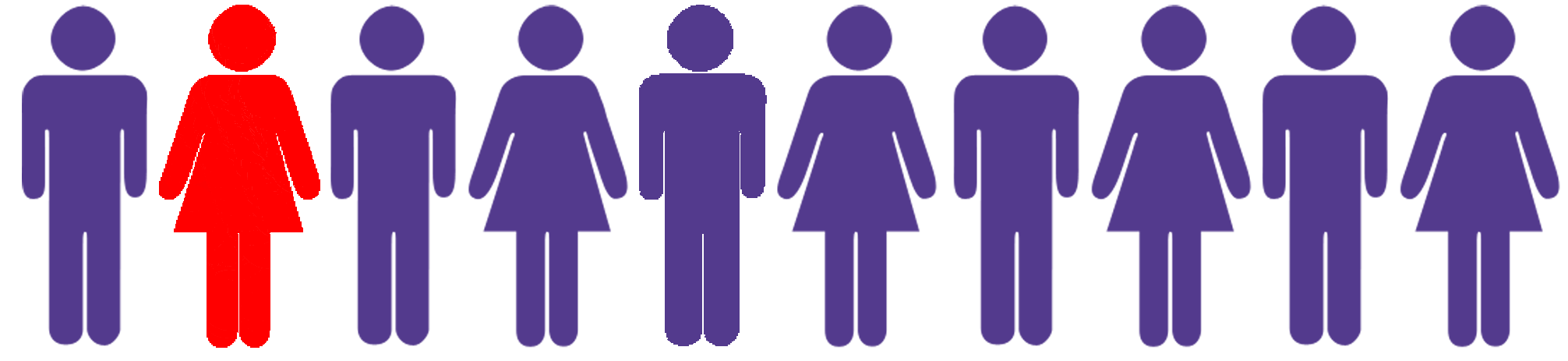
5-10% of pancreatic cancers can be the result of inherited changes.
